🚨 IMPORTANT RTLE EXAM ALERT: The Radiologic Technologists Licensure Examination in the Philippines is scheduled for December 11 & 12, 2025.
The Radiologic Technologist (RT) operates at the intersection of sensitive patient data and powerful imaging technology. Understanding ethical boundaries and legal requirements is vital for protecting both the patient and the professional license.
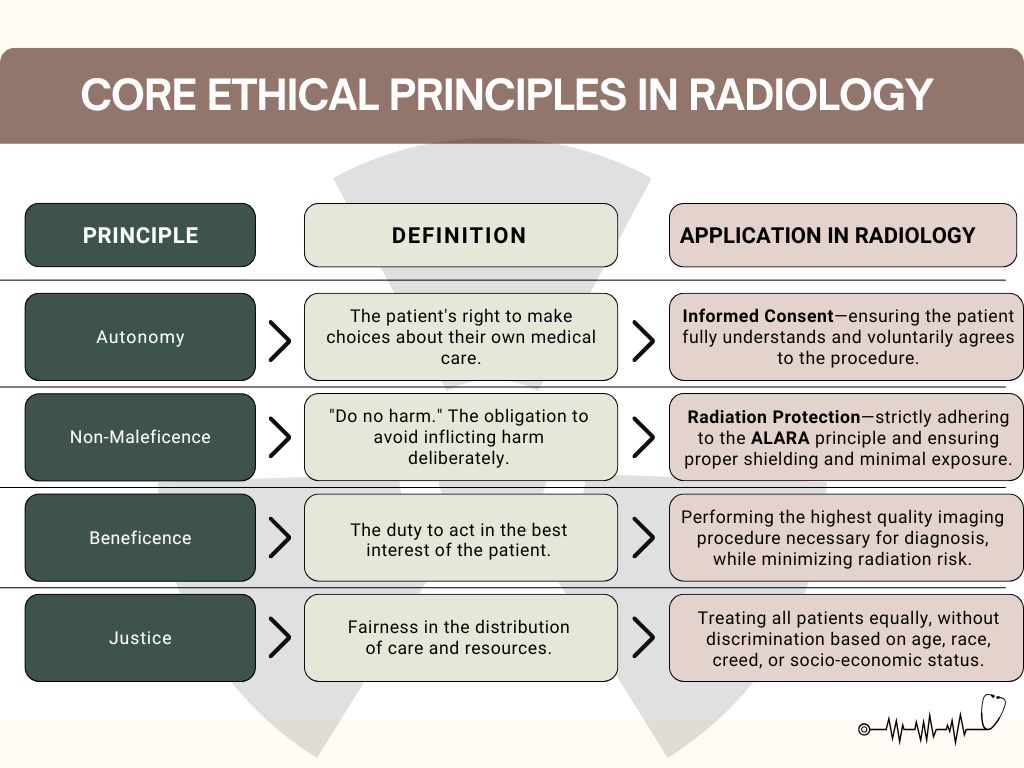
1. Core Ethical Principles in Radiology
These four principles form the foundation of healthcare ethics and should guide every decision you make in the imaging department.
2. Navigating Confidentiality and HIPAA (Privacy)
Confidentiality is the ethical obligation not to disclose information about a patient without their explicit permission.2
- What is Confidential? Any and all patient identifiers, diagnosis, images, medical history, and treatment details.
- The Law (Local and Global): While the U.S. has HIPAA, the Philippines has the Data Privacy Act of 2012 (RA 10173), which requires the protection of all sensitive personal information, including health records.3
- Practical Guidelines:
- Never discuss patient cases in public areas (hallways, elevators).
- Ensure computer monitors are not visible to unauthorized personnel.
- Do not share images, data, or personal details on social media.
3. The Cornerstone: Informed Consent
Informed consent is the process by which a patient, with sufficient understanding of the procedure, risk, and benefits, grants permission for treatment or examination.4
- Essential Components: Consent must be Voluntary (freely given), Informed (adequate explanation of the procedure, risks, benefits, and alternatives), and granted by a Competent person.
- The RT’s Role in Consent:
- Verify the patient’s identity and the correct procedure.5
- Explain the process of the exam (e.g., “The table will move,” “You need to hold your breath”).
- Answer questions about the procedure itself.
- Crucial Boundary: If the patient asks about risks, prognosis, or alternatives, the RT must defer to the referring physician or radiologist—the RT is not medically qualified to discuss these matters.
- Special Cases: Consent for minors or unconscious patients must be obtained from a legally authorized representative or surrogate.
4. The Radiographer’s Legal Boundary: No Interpretation!
This is the most critical professional boundary and a key point of ethics and law on the RTLE.
- The Principle: The RT is licensed to create the image and document the procedure, not to diagnose or provide a prognosis.
- Why? Image interpretation is the sole responsibility of the Radiologist (a licensed physician who specializes in diagnostic imaging). The RT lacks the medical training and legal authority for diagnosis.6
- Scenario to Avoid: A patient asks, “Does this look broken?”
- The Correct Response: You must maintain a professional and reassuring demeanor while strictly avoiding interpretation. A safe response is: “I am not licensed to read the images. I can confirm the image quality is excellent, and the Radiologist will review it and provide your official results to your doctor very soon.”
- Legal Basis: This division of labor is reinforced by the Radiologic Technology Act of 1992 (RA 7431), which strictly defines the scope of practice for the Radiologic Technologist.7
Mastering these ethical guidelines is essential, not just for passing the RTLE in the Philippines, but for building a trustworthy and legally sound career in the field of diagnostic imaging.